What helps with trigeminal neuralgia?
Therapies can best be classified in the following groups (from minimally invasive through invasive):
- Drug-based / conservative therapy
- Surgery
- Radiosurgical therapy (irradiation)
- Destructive procedures (percutaneous thermocoagulation)
When should a patient go to the doctor?
Trigeminal neuralgia needs to be classified and differentiated from other facial pain such as trigeminal neuropathies (after an accident), dental disease, vascular inflammation (giant cell arteritis), pseudotrigeminal neuralgia (facial pain emanating from the cervical spine). Secondary trigeminal neuralgia is targeted with specific treatment as far as possible and individual symptoms treated (with drugs) where necessary.
Similarly, drug-based treatment is initially started with classic trigeminal neuralgia despite the known cause, in order to avoid the need for surgery (see below). Carbamazepine, oxcarbamazepine, lamotrigene, pregabalin, gabapentin, baclofen, seldom phenytoin are used first, sometimes in combination. It is useful to make patients aware of local self-help groups/forums.
The countless therapeutic options demonstrate the absence of one single therapy. Each option has its own specific pros and cons. The aim must be to ascertain the best therapy for the individual patient.
If drugs become less effective over time or serious side effects from the drugs occur, the other methods can then be used.
Radiosurgical therapy
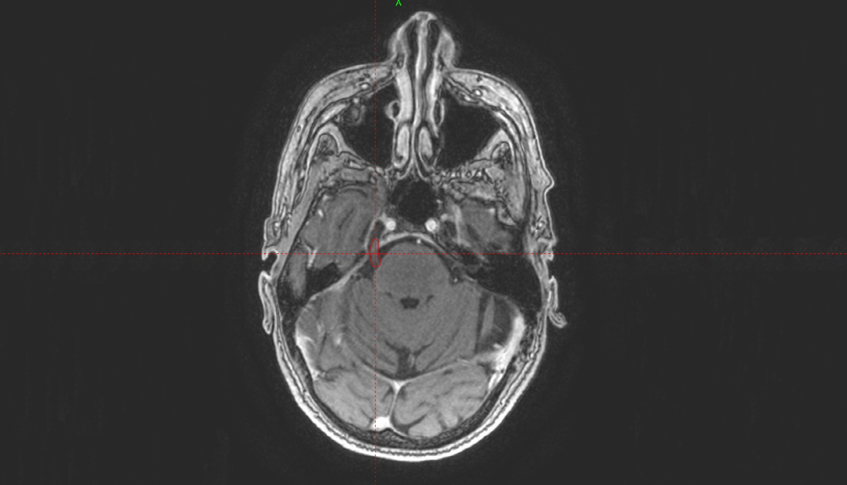
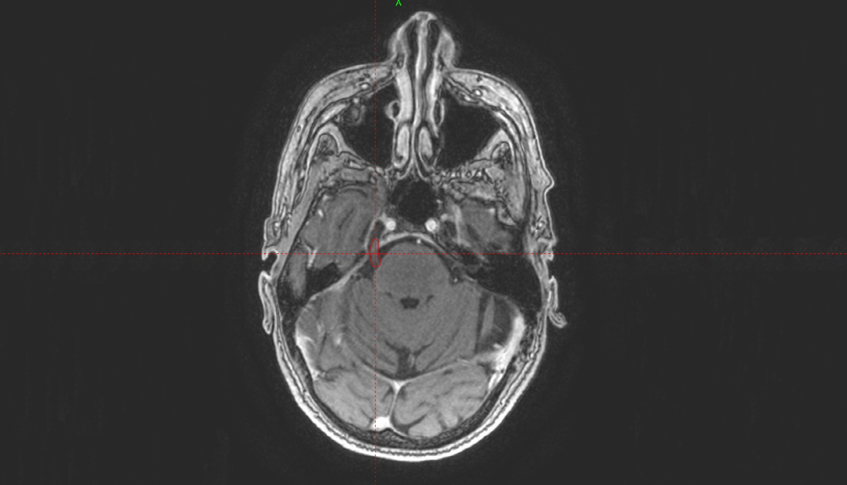
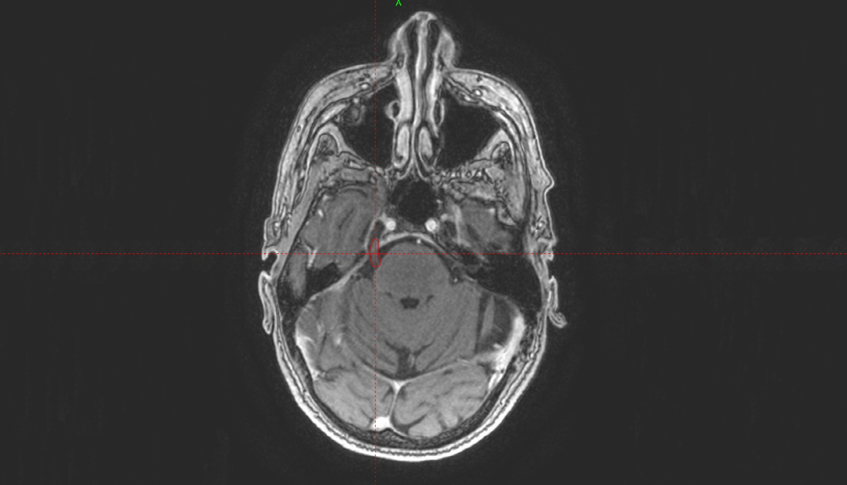
The least invasive, highly effective procedure is single-dose radiosurgery of the trigeminal nerve with the Gamma Knife. Dr. Lars Leksell, inventor of the Gamma Knife, presented successful results from this alternative treatment for the first time in 1971. The focused high-precision radiation scars the nerve in a targeted manner. To this date, we have continued to build on and improve our knowledge of this type of treatment and leveraged the continual technical improvements of the Gamma Knife and associated radiosurgery imaging techniques.
Gamma Knife radiosurgery substantially reduces the pain of trigeminal neuralgia in around 75% of cases, according to the literature. Unlike other procedures, the pain improvement is time-delayed, taking on average a few weeks to months. Around a third of treated patients may find the pain returns after a few years. They can then be given the option of repeated radiosurgery.
Factors suggesting a positive long-term treatment outcome include a short disease course under three years, no prior surgery, faster, more pronounced pain reduction after radiosurgery, and onset of facial numbness that is well tolerated by patients (compared to the previous pain).
There is often no surgical option (microvascular decompression using the Janetta procedure) when multiple sclerosis causes trigeminal neuralgia. Here radiosurgery with the Gamma Knife provides a good alternative.
Radiosurgery often improves symptoms where a tumor causes the trigeminal pain. If radiosurgery also treats the trigeminal nerve, trigeminal pain appears to be easier to manage according to the literature; results from long-term studies need to confirm this conclusion.
Undesired side effects such as anesthesia dolorosa (painful discomfort) or loss of sensation in the region of the eye are extremely rare.
Surgery
Microsurgical microvascular decompression (Janetta surgery) involves gaining access through the back of the head past the cerebellum to implant a piece of Teflon between the pulsating vein or artery and the trigeminal nerve. This prevents the vascular pulsations associated with blood pressure from being transferred to the nerves. It is the only specific therapy for classic trigeminal neuralgia. With an experienced surgeon and healthy patient, the surgery is safe. However, risks include a cerebral fluid fistula that can lead to meningitis, deafness, facial sensory deficit, facial paralysis.
Compared to other methods, surgery offers the best chance of pain reduction. It is also more enduring than other procedures and constitutes a causal therapy with neurovascular contact.
Destructive procedures
Other methods involve ablative (destructive) procedures using heat, compression, or glycerol injection. With all these procedures, a probe is pushed in the cheek up to the skull base and into the foramen ovale, trigeminal ganglion, which is located within the skull anatomically. It is lesioned specifically to reduce nerve impulse signals. This surgery is low-risk in the hands of an experienced surgeon. Risks include bleeding when injuring a vein or artery, new pain such as permanent discomfort (anesthesia dolorosa), facial numbness (common), loss of sensation in the eye with an injury to the first trigeminal branch, leading to a risk of corneal injury (foreign body in the eye goes unnoticed) and resulting loss of sight. The results have also been well investigated in the literature. Compared with Janetta surgery however, the response is lower, the reduction in pain endures for a shorter period, leading to earlier recurrence.
Personal consultation regarding therapy
A consultation with the patient should help determine the most promising therapy option. Therapies should therefore always be performed on an interdisciplinary basis in cooperation with the other physicians involved.